What is The Right Size Dental Implant?
The dental implant treatment should include the ideal implant size, based primarily on biomechanical and esthetic considerations. In traditional prosthetics, when a tooth is replaced, the abutment teeth are already provided by nature with wide posterior abutments for posterior teeth. When teeth are replaced with dental implants, the implant team should preselect the ideal abutment size, based on the ideal size for an esthetic restoration within biomechanical guidelines.
Table of Contents
How is the size of dental implant determined?
The size of an implant used to be determined primarily by the existing bone volume in height, width, and length. The surgeon would select longer implants in the anterior regions of the mouth and shorter ones in the posterior areas because of the limits of the mandibular canal and maxillary sinus. The width of the implant, also determined at surgery, would relate to the existing width of available bone, and one diameter implant (4 mm) would be used in most all situations.
Over the years, dental implant treatment plans incorporating biomechanics have been advocated to decrease the most common complications – those related to stress. The prosthesis first is planned, including whether the restoration is fixed or removable, how many teeth are replaced, and the esthetic demands. The patient force factors are then considered to evaluate the magnitude and type of force applied to the restoration. The bone density is evaluated in the regions of the potential implant placement. The key implant positions and the implant number are then selected in relation to the patient force factors and the bone density in the implant sites. For example, when the patient has parafunction or the bone is less dense or when a cantilever is present, the greater force exerted on the implant abutments will transmit greater stresses to the implant-bone interface.
The next consideration in this ideal treatment plan sequence is the implant size. Dental implants function to transfer loads to surrounding biological tissues. Biomechanical load management is dependent on two factors: the character of the applied force and the functional surface area over which the load is dissipated. The implant size directly affects the functional surface area that distributes a load transferred through the prosthesis transferred through the prosthesis. A comprehensive approach to the overall dental implant size begins with the identification of clinical problems to be addressed. Fundamental scientific principles related to force and surface area are then combined with engineering principles to pursue the desired clinical goals. Esthetic considerations in regards to implant size also are crucial to the evaluation.
In a two-stage healing protocol, the ideal implant length should be 12 mm to 16 mm. The softer the bone, the longer the implant requirements. The greater the bite force, the longer the implant dimension. Therefore, the shortest implant length may be treatment planned in the anterior mandible, the anterior maxilla should have a slightly longer implant, the posterior mandible a longer implant, and the longest implant requirement for an ideal treatment plan is usually found in the posterior maxilla.
What is the diameter of the ideal dental implant?
The diameter of the implant is also an important part of an ideal treatment plan. The diameter of an implant has a surgical, loading, and prosthetic consideration. In the initial treatment plan, the loading and prosthetic components are most important. The width of the implant is directly related to the overall functional surface area. Therefore, where the forces are greater or the bone is less dense, the implant is wider, ranging from 3 to 6 mm. As a general rule, the narrowest implant is found in the anterior mandible, followed by the anterior maxilla and the posterior mandible; the widest diameter requirements are found in the molar region of the posterior maxilla.
The prosthetic aspects of the implant width are primarily related to the esthetics of the emergence profile, the force on an abutment screw and the strength of the implant components. As a result, wider diameter implants are selected in the molar regions; standard diameters in the canines, premolars, and maxillary central incisors; and the smallest size implants in the maxillary lateral and mandibular incisors. The natural dentition follows the guidelines established in the implant size treatment plan considerations. The correlation is most likely found because of the biomechanical relationship of the amount and type of the forces in the location of the jaws and the type of the bone in the region. Therefore, in the maxilla, fine trabecular bone is used to dissipate forces. The angle of the force to the premaxilla is 12 to 15 degrees, and the amount of force is the greatest in the molar region. The mandible is a force-absorbing unit and has coarse trabeculae and dense cortical bone. The tooth size difference is reflected in the diameter of the tooth, not in the overall length dimension. These guidelines are consistent when engineering principles used in determining tooth size.
What Are Dental Implants Made Of?
In the 1960s, dental implantology as a clinical discipline was judged by some to be rather disorganized, and treatments provided were often said to be not as successful as hospital-based orthopedic and cardiovascular surgery procedures.
One part of this opinion related to the use of standard intraoral dental materials for implants plus general dental operatories for surgical activities. The biomaterials discipline evolved rapidly in the 1970s. Successful uses of synthetic biomaterials have been based on experience within the field of dental implantology.
The basis for many of the newer and more clinically successful surgical reconstructions evolved within dentistry, with some now recognized as the most successful types of musculoskeletal reconstructive surgery. That has meant that the biomaterials discipline has evolved significantly over the past decades, and synthetic biomaterials are now constituted, fabricated, and provided to health care professionals as mechanically and chemically clean devices that have a high predictability of success when used appropriately within the surgical disciplines.
Biomaterials include bulk and surface properties, and emphasis has been placed on the published literature on how these biomaterial properties relate to interactions at the tissue interface. Surface characterization and working knowledge about how surface and bulk biomaterial properties interrelate to dental implant biocompatibility profiles represent an important area in implant-based reconstructive surgery.
The literature includes summary information on surface and bulk properties for metallic, ceramic, and surface-modified biomaterials. Controlled clinical trials following prospective protocols, of course, provide the final evaluation for both safety and effectiveness. Long-term success is thus determined clinically in investigator follow-up studies and is clearly an area that should be emphasized for many available dental implant systems.
Research and development basic studies within the physical and biological sciences have been supportive of the development of surgical implant systems. One example is the continued progress from materials that have been available for industrial applications to the new classes of composites that have evolved for biomedical applications.
This same situation exists within a broad area; for example, surface science and technology, mechanics and biomechanics of three-dimensional structures, pathways and processes of wound healing along biomaterial interfaces, and the description of the first biofilms that evolve on contact with blood or tissue fluids. The progressive move from materials to quantitatively characterized biomaterials has been extremely important to the biomedical applications of surgical implants.
Titanium and Porcelain:
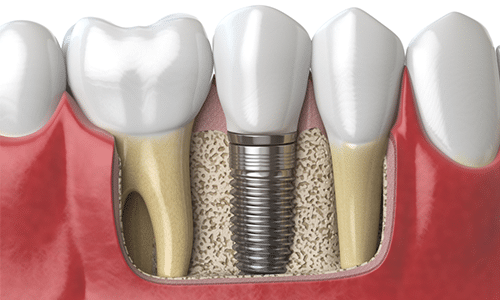
A typical implant consists of a titanium screw (looks like a tooth root) with a roughened or smooth surface. The majority of dental implants are made out of commercially pure titanium, which is available in four grades depending upon the amount of carbon, nitrogen, oxygen, and iron contained. Titanium is a biocompatible material that is accepted by the body and serves as a strong and sturdy foundation for replacement teeth. Your natural bone locks the implant into place by fusing (osteointegration), or attaching itself to the implant becomes a strong and sturdy foundation for replacement teeth.
Zirconium implants:
Zirconium is a material that can integrate with bone equally as well as titanium and its use eliminates patient concerns about metal allergies or sensitivities. Potential advantages of choosing zirconium include zero risk of corrosion and its use eliminates the possibility of metal showing through the gums or becoming exposed due to gum or bone recession. Zirconium Implant is also thermally non-conductive but it is debatable if a person could actually feel thermal conductivity from a titanium implant. Zirconium has been in use for a relatively short period so its potential for longevity is not yet proven and less is known about the way it is osseointegrated.
Zirconium implants are made as one piece incorporating the post and the abutment which leaves very little room for error. Healing can be more complicated because the implant cannot be buried underneath the gum tissue and any movement could impede fusing with the bone. The implant must be surgically placed at the correct location and angle, and bone volume is critical. Often where bone volume is less than optimal, it is possible to place a titanium implant and a bone graft at the same time, a procedure that would be riskier with a zirconium implant. Zirconium implants, particularly smaller diameter implants, may not be the best choice for patients with heavy function as they have been known to fracture.
The most popular implant components are made of titanium or a titanium alloy, and there are now many people worldwide who have had their titanium implants for many years. That said, some people do have sensitivities or metal allergies and do not wish to take any chances with their implant treatment. For patients in this position, zirconium can be a good option when used in the right clinical situation.
-
December 09, 2021Dental Implant Cost & Care
-
October 04, 2021Full Mouth Dental Implants Cost and Procedure
-
September 16, 2021Dental Bone Graft Cost, Materials and Procedure
-
June 15, 2021What is the average cost of Snap on?
-
May 27, 2021A Complete guide to Dental Implants Process and Timeline
-
May 10, 2021What Can You Do for Missing Teeth?
-
May 09, 2021What is The Cost of Single Tooth Implant?
-
January 17, 2021Do I Need Medical Clearance Before Dental Surgery?