Temporomandibular Joint Disorders

Table of Contents
Have you ever heard of TMD?
Some of you have heard about TMD (Temporomandibular Joint Disorders) and can link it to very bad facial pain. Those of you who have been diagnosed with TMD know the symptoms and the signs and are very aware of what it is but for those of you who don’t this guide is for you.
TMD is known as temporomandibular disorders. Most of the time it gets mixed up with TMJ which means temporomandibular joints. TMJ joints are located on each side of your head and are in conjunction with your muscles, ligaments, disc bones and enable you to speak and yawn. Although these joints are included in TMD they are not to be mixed up or mistaken for the same disorder. TMD occurs when your temporomandibular joints are not working properly.
Chronic facial pain, jaw pain, headaches, and earaches can be felt by more than 15% of the American population. The pain is more common in women than in men and mostly occur among people the ages of 20-40. TMD is the cause of this type of pain and discomfort which can be temporary, or it can last for years.
What causes TMD?
No one really knows the exact cause of TMD but what is really known is that the symptoms come from problems within the muscles of the jaw and with parts of the joint. This can be linked to grinding and clenching your teeth, stress that provokes you to tighten your facial muscles and jaw, dislodging the disc between the ball and socket, osteoarthritis or rheumatoid arthritis in the TM joints and injury that occurs to your jaw, neck or head.
How does TMD get diagnosed?
In order to diagnose someone with TMD your oral surgeon will have to check your TM joints for any signs of tenderness or pain. They examine you for things that involve locking your jaw and analyzing your bite. Your dentist will listen for a clicking or popping sounds as you move your mouth. In some cases, you will have to have a panoramic x-ray taken and your dentist may refer you to an oral surgeon for treatment.
What are the symptoms?
Symptoms include facial, neck and shoulder pain when you chew, speak or open your mouth widely. Sometimes you might have an inability to fully open your mouth, your jaws may be locked, you may have difficulty chewing and discomfort when biting, dizziness, earaches, hearing loss, toothaches, headaches or neck pain. Two of the most common symptoms are swelling on the side of the face and clicking or popping sounds when your jaw is closing. It is common to experience pain when this happens. Sometimes there will be no payment involved. In the event that you feel any of these symptoms, it is imminent to call your dentist for treatment.
If you experience TMD pain it is recommended that you limit any discomfort in your face and jaw. It is best to talk to your dentist about pain medication such as ibuprofen or any other low-grade over-the-counter medicine. Eating soft foods as much as you can help. It also helps to avoid strenuous activity such as lifting and exercise. This prevents you from becoming overstressed. When you’re overstressed you tend to clench your teeth and agitate your TMD muscles and joints.
Once you know that you have TMD pain it is time to seek treatment as soon as possible. If TMD is left untreated it can cause complicated problems that pose a significant risk to your health such as poor oral health, chronic headaches, lack of sleep due to teeth grinding, malnutrition, eating disorders and hearing problems.
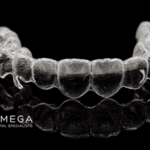
If you are diagnosed with TMD your dentist or oral surgeon might recommend that you use a splint or a night guard. A splint or a night guard is ideal for those who have TMD. A splint or night guard acts as a mouthguard during the night time when you sleep. It can help to fight grinding of teeth and clenching your jaw while you’re sleeping or under stress. Here are a few other treatment options that your dentist or oral surgeon would recommend:
Transcutaneous electrical nerve stimulation:
Transcutaneous electrical nerve stimulation (TENS) is a type of therapy that involves low voltage electrical currency for pain relief. This involves a small machine that is battery powered and is the size of a pocket radio. With this machine, you connect two wires that conduct electrical currency from the machine to your skin. This device is completely safe when used properly and safely according to instructions given.
Trigger-point Injections:
Trigger point injections are used with local anesthesia so that the injection site is less tender. Trigger point injections treat jaw muscle pain and can treat various elements such as fibromyalgia tension headache and myofascial pain syndrome. The way that this injection works is that the medication is injected directly into the trigger point. The trigger points are the upper back and around the shoulders which are typical focal areas of the muscles.
Teeth Correction: Getting your teeth corrected can be an effective treatment for TMD. Teeth correction can span from jaw surgery or braces whichever option you prefer and have spoken to a dental professional about. Think teeth correction is right for you. Schedule a visit at Omega Dental Specialist to speak to one of our trusted oral surgeons regarding TMD pain and treatment options.
Is my jaw dislocated?
There is a joint that connects the skull and the jaw that is known as the temporomandibular joint. Positioned just in front of the lower part of the ear, the temporomandibular joint is considered a ball and socket type joint. This is similar to joints found in other parts of the body such as in the hip or the shoulder. When the mouth is opened wide, the ball portion of this joint comes out of its socket, and when the mouth is closed, it returns. A dislocation of this jaw joint happens any time the ball portion of the joint pops out too far from the socket. When it does not return to its normal position in the socket, the patient has experienced a dislocated jaw.
What causes spasms in the TMJ?
This particular type of event usually happens when the ligaments associated with the joint become too loose and ultimately are incapable of positioning the ball joint back into its normal resting place. A dislocation may also occur anytime patients experience joint spasms that will not allow the ball portion of the joint to return to its position normally. Further, any traumatic injury that causes the jawbone or joint to fracture or break results in similar results. In fact, anything that causes the jaw joint to unhinge from the skull is known as a dislocation. As discussed, this can occur through injury or can be muscle related.
Helping Your Temporomandibular Joint Heal
A dislocated or broken jaw can be a serious concern because it ultimately causes varying levels of chronic pain as well as problems with eating and normal breathing. In most instances, emergency medical attention is recommended as a way to minimize any complications associated with this type of dental distress. Most importantly, fast and responsive medical attention can help to accelerate the healing process. While weakened muscles are often responsible for a dislocated jaw, there are some facial trauma-related events that can also result in a dislocated or broken jaw. For example, a slip and fall accident or an accident in the workplace can easily cause a jaw injury or dislocation.
TMJ Swelling And Persistent Pain
Also, those actively involved in sports or anyone who has been involved in a vehicular accident may experience a dislocated jaw. Even something such as a physical assault that involves the face or head region may end up triggering a dislocated or broken jaw. While there are certainly some symptoms that can be associated with a broken or dislocated jaw, there are some that are more common than others. For example, one of the most obvious signs that the jaw has been dislocated is a swelling and persistent pain. Bleeding is another obvious indicator that an individual may have a broken jaw.
Excessive Blood Flow
In more extreme cases, the entire face can become swollen while the jaw may become stiff and immobile. Bleeding from the mouth is a major concern while difficulty with breathing is equally as serious. This is especially true considering the fact that excessive blood flow can end up blocking an individual’s airway. Pain may often be most noticeable when chewing or speaking. In other types of extreme cases, the jaw may be completely immobilized making it impossible to move it even slightly. Also, those with a broken or dislocated jaw could have facial bruising or numbness of the gums.
Dislocated Jaw
It should also be noted that a dislocated jaw does often have different signs or symptoms as compared to a broken jaw. Some of the more common signs associated specifically with a dislocated jaw include an excessive or very obvious overbite. If the teeth do not line up normally or if an abnormal bite is experienced or it is impossible to completely close the mouth, it is more than likely that a dislocated jaw is involved as opposed to a broken jaw. There are some treatments that are used to address jaw injuries. In most cases, these treatments are considered emergency in nature and should be given priority.
Treating a dislocated jaw involves the doctor placing the jaw back into its normal position. This may be done manually while in other cases muscle relaxants along with anesthesia can assist in making the procedure easier for both the doctor and the patient. In some situations, surgical procedures may be required to correct a dislocated jaw. This is also true when talking about a broken jaw where surgery is commonly the best option for the patient. That said there are also many cases where clean breaks will heal effectively on their own.
Severe TMD Treatment
As an added note there are some types of dislocated jaw conditions that are best handled by simply wiring shut the jaw. The wire is used as a way to help promote healing so that the healing process will not be interrupted. Both wires and elastic bands can be used for this purpose. It takes time to recover from a dislocated or fractured jaw. Patients should keep this simple fact in mind and that it will be difficult to open the jaw for the first several weeks during initial recovery. Talk with your dental care provider to determine if you have a dislocated or broken jaw.
If you have any question or concern about facial pain and temporomandibular joint disorders, contact us to make an appointment with one of our specialists.
Related articles:
- 10 Things You Need to Know About Dental Implants in Houston
- What you need to know about Omega Dental Specialists Implant Center
- DENTAL IMPLANT BENEFITS
- ARE DENTAL IMPLANTS RIGHT FOR YOU?