Failed Root Canal Symptoms

A failed root canal is a common dental problem that needs immediate attention. Root canal therapy is a minimally invasive treatment. It helps to clean the root canal system infection, decrease pain, and preserve patients’ natural teeth. Dentists perform Millions of root canals every year with a very high success rate. In addition, the vast majority of patients are satisfied with the treatment and outcome of this safe procedure.
However, as in all medical and dental procedures, there’s a slight risk of root canal therapy failure. When this happens, it’s essential to recognize the signs, symptoms, and causes. Fortunately, endodontists can mediate a failed root canal with retreatment and surgical options. Let’s take a closer look.
Table of Contents
What are the Reasons for Failed Root Canals?
Days, weeks, months, or even years after root canal therapy, a patient can discover that their initial root canal didn’t heal properly. Recent trauma or decay can compromise the root canal area once again and can cause infection. In the majority of cases, one of these issues causes root canal failure:
– Coronal seal breakdown
After a root canal, the endodontist or your general seal the coronal part of the root canal system. They seal it by a permanent restoration to protect root canals from further infection. If this coronal seal breaks down, the tooth is once again vulnerable to bacterial leakage and can become re-infected. To prevent
– Crown breakdown leading to failed root canal
When the endodontist place the crown, that protects the tooth, too late after the procedure, bacteria can re-enter. This is also possible if the crown breaks or is cracked by an injury. We always recommend the patient to go back to his/her general dentist as soon as possible to place to restore to the treated tooth with a permanent restoration. Your dentist may recommend a crown for root canal-treated posterior teeth.
– Failure to clean the canal
If the canals are too narrow, curved, or have a complex system, it makes it hard and sometimes impossible to clean the root canal system. In other cases, the original dental x-rays don’t show cracks or resorptions in the tissue that could harbor bacteria. If the canals weren’t adequately cleaned, the infection could easily recur and spread.
– Decay or trauma leading to Failed Root Canal
In some cases, the root canal becomes compromised due to a new tooth injury or tooth decay that once again exposes the tooth’s sensitive tissue to infection.
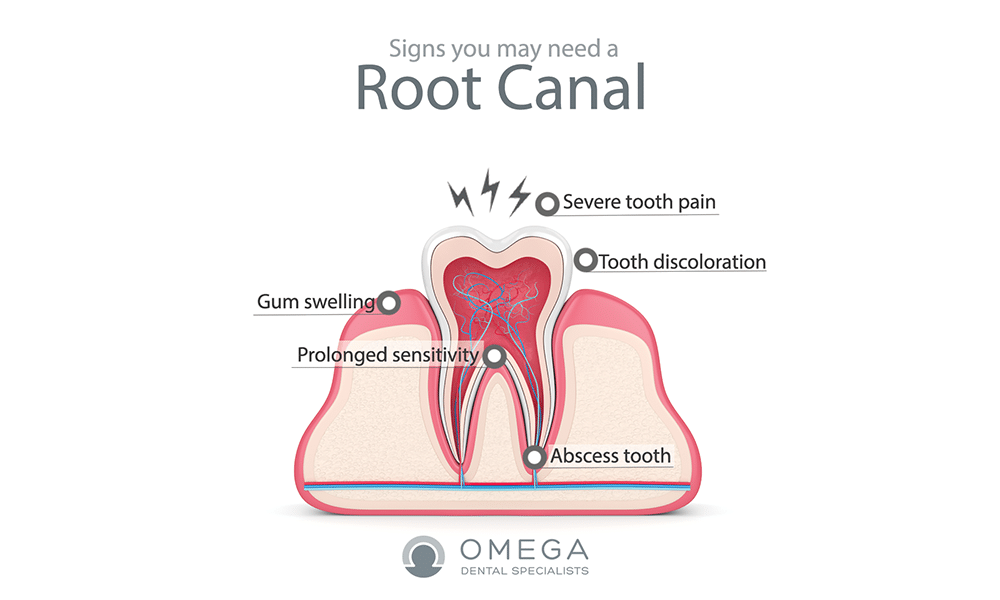
What are the signs of root canal failure?
Whether you had a root canal 12 weeks, 12 months, or 12 years ago, it’s important to keep an eye on your dental health. If you start experiencing signs of root canal failure like pain, swelling, discharge, or a boil on your gumline that won’t go away. It’s important to seek treatment. Feel like you may be experiencing a failed root canal? Get in touch with your local team of endodontists today.
Root canal complications are serious and you must see your dentist immediately. Whether your root canal was performed months or even years ago, you may be feeling that something isn’t quite right. Perhaps you’re experiencing root canal pain that comes and goes near the affected tooth. Or maybe you’ve noticed that you’re suddenly more sensitive to heat and cold than before.
In many ways, signs and symptoms of root canal failure are similar to the sensations that may have motivated you to seek the procedure in the first place. When root canal therapy heals like normal, the patient will usually experience a drastic reduction in pain. A failed root canal, however, will result in the same symptoms that highlighted the need for a root canal in the first place.
Signs of root canal failure:
- Pain in the tooth after a root canal
In a root canal that heals properly, pain should normally dissipate after only a few days. However, in the case that bacteria have re-entered the canal, you will likely experience severe pain in the infected tooth.
-
Swelling
As the infection takes hold, you will often experience swelling as well.
-
Discharge
In some cases, you will experience discharge from the affected tooth. This could indicate that an abscess has formed due to the infection.
-
Increased tooth sensitivity
In some cases, this could mean you are more sensitive to heat or cold; for example, you might find it unbearable to eat ice cream or sip hot soup. In other cases, you might be more sensitive to any pressure – like when you eat or press teeth together.
-
Boil or pimple on the jaw
If you’ve noticed a boil or pimple on your jaw that won’t go away, your body might have established a sinus tract with the intent to drain pus associated with an infection.
-
Maxillary Sinusitis of Endodontic Origin
In some cases, infections in your back teeth can spread into your maxillary sinus. When this happens, you’ll experience sinus issues like runny nose, congestion, stuffiness, facial and jaw pain, and bad breath.
-
Tooth Discoloration
If you’ve noticed that the tooth is darkening or changing in appearance, it may be a sign to get it checked out.
-
No symptoms at all
In some cases, you may experience root canal failure with no pain, swelling, or other symptoms. Your first inkling that something is wrong may come from a routine x-ray at your dentist’s office — which is why it’s so important to stay up-to-date with your dental appointments.
Why Do I Need Root Canal?
In cases of injury or decay, bacteria can get inside the tooth’s root canal and cause infection and inflammation. When this happens, you need root canal therapy — an endodontist cleans the pulp (and any infection) from the root canal, fills the canal with a rubber-like material, and seals the space off to prevent further infection.
Initially, root canal therapy is generally necessary when tooth trauma, injury, or decay has exposed the soft pulp within the “root canal” of the tooth. Once exposed, the pulp is vulnerable to bacteria, which causes infection and inflammation. As the infection progresses and spreads in this nerve-rich tissue, it can cause severe pain and swelling. Additionally, the infection can weaken the surrounding tissue and lead to damage to your jawbone and gums — eventually leading to tooth loss.
During an initial root canal, your dentist or endodontist accesses the soft inner tissue of the tooth through the crown of your tooth. Then, they remove the infected pulp, disinfect the area, and seal it to prevent further infection. Often, though you retain your original tooth, the practitioner places a crown over the area to protect it further.
Why do I need another root canal treatment?
However, as with all medical procedures, there is a slight chance of failure when it comes to root can When this happens, it’s important to recognize the signs that something is going wrong — and understand your options for treatment. Seeking a qualified endodontist — a professional who specializes in root canal treatment — is the first step when a root canal goes wrong.
If your root canal treatment has failed, you might need another endodontic procedure. In most cases, seeking root canal retreatment can help save your tooth, decrease your root canal pain, and prevent the infection from spreading. Without adequately addressing the root of the problem, it’s likely that your symptoms will increase — and you may lose the tooth. Here’s what to expect from root canal retreatment:
- First, your endodontist applies a local anesthetic and re-opens your tooth. They may have to remove the crown that’s in place, and will also remove the canal filling within the tooth.
- Then, they’ll meticulously clean the inside of your canals. At this point, they’ll be sure to assess the inside of your tooth very carefully, ensuring that any narrow, curved, or irregularly placed canals are thoroughly cleaned.
- Finally, they will fill and seal the canals and place a temporary filling to protect the area. You’ll have to return for a crown as soon as possible to prevent the risk of re-infection.
Root Canal Surgery: An Alternative to Retreatment
In some instances, your endodontist might recommend that you get root canal surgery instead of root canal retreatment. You may need root canal surgery in some of the following situations:
- To locate small fractures or canals that x-rays can’t catch during the initial treatment.
- Remove calcium deposits in root canals.
- To treat damaged root surfaces or bone.
- Remove inflammation and infection around the root.
One of the most common root canal surgeries is an apicoectomy or root-end resection. Using a local anesthetic, your endodontist ensures that you will feel no pain or discomfort during the procedure. With the latest and most innovative technology, your endodontist then uses micro-surgery techniques to open the gum tissue near your affected tooth.
From there, they can easily remove any infected or inflamed tissue. Additionally, they will remove the very end of the root, sealing the area with a small filling and placing sutures or stitches. If the bone has been severely damaged, they may need to utilize bone grafts to promote healing. In general, patients return to their everyday lives just a day after the surgery. Over the months, your bone will heal around the end of the root.
What are the Alternatives to Endodontic Retreatment and Endodontic Surgery?
An untreated failed root canal is a severe infection. It can form a painful and dangerous abscess, and in some cases, even lead to a septic infection. When it comes to infected pulp tissue, if you choose not to have endodontic retreatment or surgery, your only option is to extract the infected tooth. Though it’s preferable to keep your original tooth, if possible, an extraction followed by an implant is sometimes the only appropriate course of action.
Once your dentist extracts the tooth, your best choice is to have a dental implant that will mimic the look and feel of your natural tooth. Depending on the tooth, the cost of a dental implant is between $1,500 and $6,000. Additionally, the extraction itself can cost $50-900per tooth.
Frequently Asked Questions About Root Canal Failure
If you think you may be experiencing root canal failure, you probably have many questions. Although everybody’s situation is entirely different — and it’s best to consult your team of dental professionals — here are some brief answers to FAQ’s about root canal failure that may be helpful:
How Often Do Root Canals Fail?
Out of the whopping 15 million root canals that are given every year — which equals 41,000 performed every day in the United States — an impressive 89% of those patients report being satisfied with the work their endodontists do. Multiple studies have been done to assess the success rate of the initial root canal. One study published in ISRN Dentistry determined that endodontic treatment is successful in 86% of cases.
However, success rates can vary based on the type of oral health professional who does the treatment. For example, one 2004 study found that root canal treatment was successful 98.1% of the time when endodontists perform it, but only 89.7% successful when general dentists perform it. Overall, root canal treatment is successful, approximately 90% of the time.
How Much Does It Cost to Retreat Failed Root Canal?
Getting treatment for a failed root canal may indeed cost more than the initial procedure. However, this varies considerably based on your situation. For example, the cost may vary based on whether you’re treating a front tooth or a molar. And when it comes to having a crown replaced, the material used — porcelain, metal, ceramic, etc. — will change the overall cost. Talk to your provider about financing the procedure, or check in with your insurance company to see what they cover.