What is A Dry Socket?
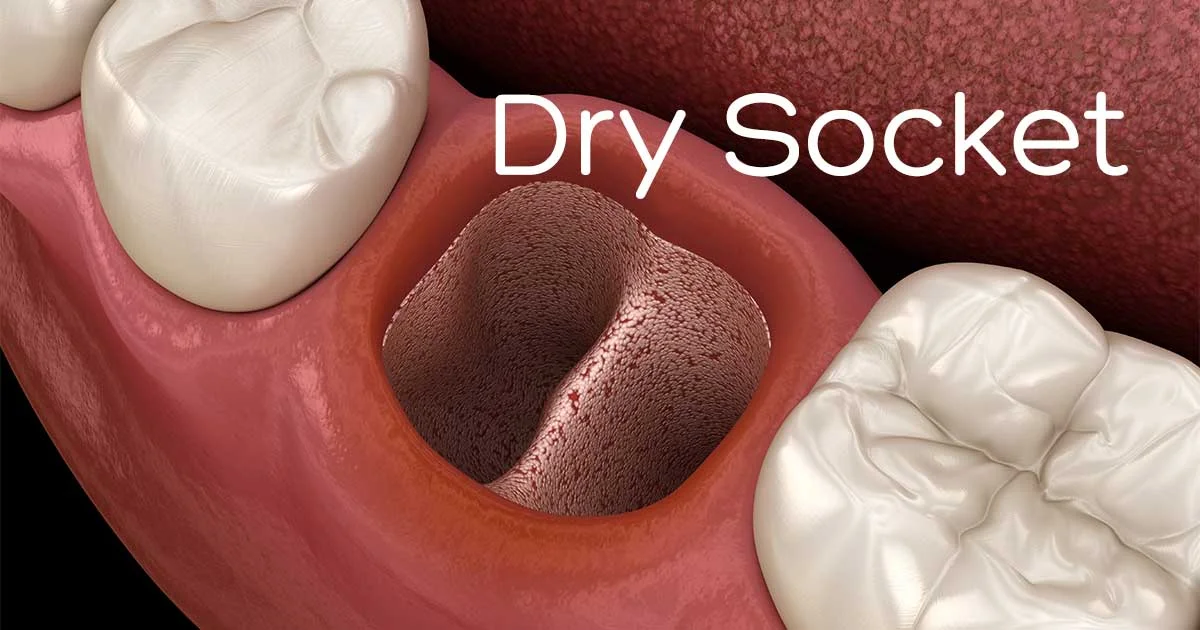
Table of Contents
What is a Dry Socket (alveolar osteitis)?
Also known as alveolar osteitis, a tooth extraction dry socket is a condition that occurs when a blood clot fails to develop in the gum tissue or does develop and then either becomes dislodged or dissolves after an individual has had a tooth extracted. This dental phenomenon affects about 2 percent and 20 percent of adults who have had non-third molars and third molars extracted, respectively. That said, no matter what tooth an individual has had extracted, if it results in a dry socket, agonizing pain is almost sure to follow. And this has a lot to do with the fact that, without a blood clot taking form and remaining intact, the bone that previously held the extracted tooth in place becomes exposed. A dry socket is caused when there is an interruption of normal healing after a tooth is removed: in normal cases of healing, a blood clot is formed where the tooth lived, to protect the jawbone and promote healing. When something happens to that blood clot or it never forms, the bone is uncovered, resulting in a painful dry socket.
How is Dry Socket Treated?
The treatment for a dry socket is usually time and symptom management. The dentist will clear the affected area and make sure food is not in the opening. Then, he or she will pack the wound, often with pain relieving medication on the dressing. Usually, pain relievers or narcotics are prescribed to manage the symptoms during the period of healing.
An Overview of Dry Socket
Dry socket is known as a dental condition that happens after a tooth removal. Dry socket is a painful thing to have. Dry socket can happen when there is a blood clot where the tooth was removed from. When it fails to develop it becomes dislodged before the wound has had time to heal. Usually, a blood clot will form where the tooth was taken from. The blood clot acts as a protective layer over the bone in the nerve endings that are within the empty tooth socket. In other words, the blood clot becomes the foundation for the development and growth of new bones and soft tissue.
When dry socket happens, the underlying bone becomes exposed along with the nerves that connect to the side of your face. This causes intense pain in the socket as well as the side of your face the removed tooth is on. The pain can be increased by food buildup within the socket as well as inflammation. If you had a tooth that was removed, you may not begin to feel this pain until one two three days after the tooth was removed indicating that you have developed dry socket. Dry socket can be frustrating to deal with because it is the most common complication followed by tooth extractions such as after the removal of the third molars also known as the wisdom teeth or the removal of permanent teeth in adults. But what can you really do about the pain? You may be tempted to visit your local pharmacy and pick up an over the counter medication to treat the pain. As easy as it is to obtain over the counter medications these types of medications will not be enough to treat dry socket pain. It is best to visit with a trusted dentist or oral surgeon that can offer you treatment to relieve your pain.

What are the symptoms of dry sockets?
The symptoms of dry sockets include severe pain that you get after a few days after a tooth was removed or extracted. The most common symptom of a dry socket is a loss of blood clot at the site of tooth extraction you will notice that it looks like its name an empty, dry socket. It is common to have partial blood clot loss at the site. You may also experience a bone in the socket that is visible, pain that radiates from the socket to your ear/eye/temple/neck that happens on the same side of your face as the extraction, bad breath, and unpleasant taste in the mouth.
Dry Socket Complications
Despite their best efforts and closely following the recommendations of a licensed dentist or oral surgeon, some individuals will, unfortunately, still develop dry sockets anyway. And along with everything mentioned so far, having a dry socket causes some of the following complications and symptoms as well:
- Severe halitosis
- A foul-tasting mouth
- The appearance of visible bone tissue in the oral cavity
- Excruciating pain radiating from the extraction site
Much like the enumeration of dry socket causes, this article details only a few of the complications and symptoms that are usually synonymous with a dry socket. To learn about others and to also discover ways to prevent dry sockets from occurring in the first place, it would be a good idea to speak with a licensed dentist or oral surgeon.
When should you see an oral surgeon?
There’s a certain amount of pain that that comes about after a tooth extraction. The amount of pain that you feel afterward should be tolerable. Tolerable means that the pain lessens with the usage of over the counter medication. If an intense pain and dry socket symptoms come about you should consult with your doctor about treatment methods immediately.
Who is Likely to Get Dry Socket?
Dry socket occurs to those who have recently had a tooth extraction. Chances of a dental patient getting dry socket are only about 2%, but they are 20% for patients who have recently had their lower wisdom teeth removed. There are a few factors that increase a patient’s chance of getting dry socket:
- Gum Disease
If the patient has periodontal disease before extraction, this can affect the mouth’s ability to form a healthy clot. Also, the presence of certain bacteria can cause erosion of the clot.
- Smoking (Nicotine use)
Smokers are more likely to get dry socket because nicotine affects the mouth’s blood supply, which can inhibit clot formation.
- Carelessness
Patients who have undergone a tooth extraction, especially of their wisdom teeth, are instructed to be extra careful while eating and drinking. The use of straws is usually warned against, as the airflow can disrupt the blood clot. Practices like spitting or over-rinsing can cause the clot to become dislodged as well.
- Hormones
Women are more likely to develop dry socket than men, due to more hormonal variations or the use of birth control pills.
- Age
Patients over the age of 30 are more likely to develop dry socket because of the breakdown of the jawbone and decreased blood supply.
What are some causes of dry socket?
There are two possible causes of a dry socket that are currently under study by researchers. In certain issues, dry socket can be caused by contaminated bacteria on the socket and trauma at the surgical site that comes from a difficult extraction procedure such as an impacted wisdom tooth.
What are the risk factors for dry socket?
Risk factors that can increase your risk of dry socket include smoking and tobacco use. Due to the chemicals in cigarettes that prevent and slow down the healing process they also can contaminate the wound site and physically dislodge the blood clot prematurely. Oral contraceptives have a high estrogen level and can disrupt the healing process and increase the risk of dry socket. Improper at-home care due to the failure of following proper home care guidelines. Poor oral hygiene can drastically increase the risk of dry socket. If you have had a dry socket in the past you’re more likely to develop it after another tooth extraction. If you have a tooth or gum infection whether current or previously, the extracted tooth can increase the risk of dry socket.
Can any complications arise because of a dry socket?
The complications that can arise due to dry socket include delayed healing, infection of the socket and progression due to chronic bone infection is also known as osteomyelitis.
How can you prevent dry socket?
You can prevent dry socket by seeking a dentist or oral surgeon who has experience in tooth extractions. It is also helpful to stop smoking before your extraction procedure because smoking and using other tobacco products can increase your risk of dry socket rapidly. You can also talk to your doctor or your dentist about programs to helping you quit for good. You can also talk to your dentist or oral surgeon about any prescriptions including over the counter medications that you’re taking. They can interfere with blood clotting and it is worth mentioning.
Preventative measures are also taken by a dentist or oral surgeon. They take several steps to prevent dry socket including having you use an antibacterial mouthwash immediately before or after surgery. It is also common for them to give you a gel as a substitute for mouthwash. Oral antibiotics may be taken if you have a compromised immune system. There may also be an antiseptic solution that gets applied to the wound along with the medicated dressing that gets applied after the surgery.
What are some of the things that you can do after surgery to prevent dry socket?
Your dentist or oral surgeon will provide you with a set of instructions about things to expect during the healing process after tooth extraction. They also give you tips on how to care for the wound along with proper at-home care. Proper at-home care helps to promote healing and it prevents damage to the wound. The at-home care instructions will address a couple of issues that can help prevent dry socket. Here are a few tips of what you can do after surgery:
Manage your activity level after your surgery. You should plan to rest for the rest of the day. Follow your dentist or oral surgeon’s recommendations about when to go back to normal activities. It’s also recommended to ask how long you should avoid rigorous exercise that might result in this lodging the blood clot in the socket.
Manage the pain. It helps to put cold packs on the outside of your face on the first day after the extraction takes place. The day after you should consider applying warm packs to the face. This helps to decrease any pain and swelling that arises. Be sure to take pain medication as prescribed.
Be cautious when consuming beverages. Drink plenty of water after surgery to stay hydrated. After the surgery, avoid any alcoholic, carbonated, hot or caffeinated beverages. Be sure that you do not drink with a straw for at least a week because of the sucking action which can dislodge the blood clot.
Soft foods should be consumed such as yogurt and applesauce on the first day. Be cautious when consuming cold liquids and biting your cheek until the anesthesia has completely worn off. You can start by eating semi-soft foods whenever you can tolerate them. Avoid chewing on the side of the mouth that the surgery was on.
Extra care should be taken when cleaning your mouth after the surgery. You can gently rinse your mouth and you can brush your teeth as long as you avoid the extraction site for 24 hours. After the first 24 hours, you can gently rinse your mouth with warm salt water several times a day for a week. You can do this by mixing 1/2 teaspoon of table salt in 8 ounces of water.
Eliminate your tobacco use. You don’t have to eliminate your tobacco use completely but do not smoke or use tobacco for at least 48 hours after surgery. It helps not to use tobacco for as long as you can. Any use of tobacco products after oral surgery, in the first 48 hours, can delay healing and increase the risk of complications including dry socket.
Need to have a tooth extracted ? Contact Omega Dental Specialist for a consultation today.
What to Do if You Have a Dry Socket?
Although the ill-effects that occur when a tooth extraction blood clot becomes dislodge or dissolves and eventually causes a dry socket, not to mention pain and other complications, there are dry socket treatments that can provide some much-needed relief. And they also go a long way toward ensuring a healthy socket after extraction. Some of these treatments, which can benefit those who have had their third molars or other teeth extracted, include the following:
Eating softer foods – Consuming soft foods, such as yogurt, applesauce, and pudding, eliminates the need to bite down or chew as forcefully, which allows dislodged or dissolved blood clots to start forming again.
Sleeping in an optimal position – Another way to combat the ill effects of a dry socket is to sleep with your head propped up on one or two pillows. Doing so improves blood circulation and, similar to consuming softer foods, allows new blood clots to form on the gum tissue.
Oral hygiene – Even though your gums are still tender, you will want to continue to floss regularly and brush your teeth twice per day. These essential wisdom teeth removal recovery tips recommended by dentists, oral surgeons, and even hygienists can help prevent a dry socket by keeping the oral cavity as clean as possible. Further, regular brushing and flossing lowers the risk of gum infection and facilitates the development of new blood clots.
Rinsing with a warm saline solution – Just like brushing and flossing, rinsing your mouth out a few times each day with a mixture of warm water and salt can help keep gum infection at bay while allowing new blood clots to take form.
Taking medication – To ease the pain associated with a dislodged or dissolved blood clot, you will want to take pain relievers as prescribed by your dentist or oral surgeon. Similarly, taking over-the-counter ibuprofen as directed can also help provide some much-needed pain relief.
January 30, 2023What to Expect During the Wisdom Teeth Extraction
October 23, 2022Wisdom Tooth Removal Cost
- July 26, 2022
Should I Have My Wisdom Teeth Removed Before I Get Braces?
July 26, 2022Complete Guide to Wisdom Tooth Removal