Gum Disease in Houston
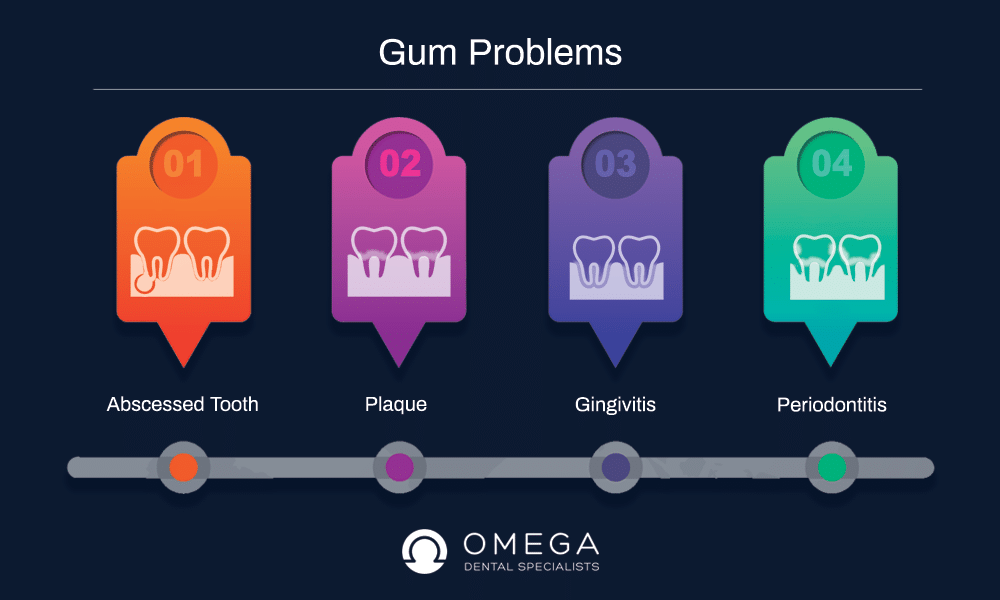
Table of Contents
What Is Gum Disease?
Gum disease is also called gingivitis or periodontitis, depending on the stage of the disease. Gingivitis is the first stage of periodontal disease. During this stage of the disease, the gums become inflamed, red and bleed. Sticky, colorless films of bacteria, plaque, are responsible for causing the symptoms one experiences with gingivitis.
Periodontitis is a serious gum infection. Periodontitis damages the gums, causing them to recede. This infection also destroys the bone that is responsible for providing the teeth with the support they need, which can cause the teeth to become loose, eventually leading to tooth loss.
What Are Signs of Gum Disease?
The Four Basic Signs of Periodontal Disease
1. Inflammation – puffy, bright red gums.
2. Halitosis – continuous bad breath (that remains even after flossing and brushing).
3. Bleeding gums – Gums that bleed while flossing, brushing or at random.
4. Receding gums – gums have pulled away from the teeth (possibly exposing the roots of the affected teeth).
What Causes Gum Disease?
Plaque is the main reason for gingivitis. Bacteria can easily live in these conditions and plaque is the perfect home for these types of bacteria. Plaque does not have a color and it is sticky and can stick to teeth. It can damage the enamel by eating away at it over time. Usually brushing your teeth brushing twice a day can get rid of most of the plaque but it doesn’t get rid of all of it. The leftover plaque that is not removed from brushing becomes hard and it turns into tartar. Once plaque turns into tartar only a dental professional that cleans your teeth can remove it. If plaque and tartar stay on the teeth without treatment, more and more bacteria can live there and multiply. This can lead to gum disease that has progressed to an advanced stage. The advanced gum disease stages are gingivitis and periodontitis.
What is Gingivitis?
Gingivitis is a gum disease, but it is milder than periodontitis. A major sign of gingivitis is swollen gums. If your gums swell or bleed easily than this is a major sign of gingivitis as well. Gingivitis is an advanced stage of gum disease, but it can be reversed by daily habits of brushing your teeth regularly, dental cleanings and routine dental visits.
What is Periodontitis?
Periodontitis occurs when gingivitis has not been treated and it becomes further advanced. Just like gingivitis, periodontists have symptoms of swelling gums. Swelling gums is usually the first sign of periodontitis. Another symptom is when gums pull away from the teeth and form pockets. When gums pull away from the teeth is known as receding gums. The receding gums form pockets that sit low in the mouth. If left untreated these pockets can make way for more bacteria to live in there as well as the development of infections. Receding gums that form pockets could speed up the teeth decaying process resulting in teeth removal. This is why it is so important to maintain your teeth and gum health. Let your dentist know if any problems occur whether it starts as something small or is a cause for concern.
Periodontal disease is caused by poor oral hygiene. The earliest stage is called gingivitis and results from the buildup of dental plaque on teeth. Red, swollen and bleeding gums during brushing or flossing are common symptoms. If left unchecked, gingivitis often develops into a more serious condition called periodontitis.
Periodontitis is an infection of the gums themselves. Plaque accumulates and hardens under the gums, causing them to pull away from teeth and expose more of the tooth to bacteria. The infection leads to bone loss around the tooth, allowing it to loosen and eventually fall out. In early stages of periodontitis there are no warning signs, and since it affects more than just the gums, it cannot be managed with daily brushing and flossing.
Sometimes the stresses of life can lead us to neglect our oral hygiene and sometimes you just simply let your oral health go. Abscesses in teeth in other gum diseases can be prevented easily if you just maintain your good oral hygiene. If you neglect your oral hygiene do not feel bad because even those who brush and floss every day religiously still experience these problems. These problems are common and can be fixed under the advisory of a dental specialist. The problem generally results from food that has not been brushed or pitch off by cleanings over time which can lead to swollen gums bleeding gums persistent bad breath, halitosis, and loose teeth.
What matters most is how you deal with the issue. Ask your dentist or specialist about how you can achieve good oral hygiene and ask about a routine in place to get started. Be sure to visit the dentist every 6 months as a routine these visits guarantee that gum disease is at bay and that plaque and tartar are regularly removed. It also helps to detect in the early stages if there are any other dental problems that you may have.
Types of Gum Disease
1. Chronic Gingivitis – causes the gums to turn red, become inflamed and bleed easily. This is the most common type of gum disease that children develop; however, chronic gingivitis can be prevented by practicing good oral hygiene. If not addressed, chronic gingivitis may lead to more serious forms of gum disease.
2. Aggressive Periodontitis – mainly affects an individual’s incisors and first molars. This disease may develop in healthy teenagers and young adults. Aggressive Periodontitis is characterized by a severe loss of the bone responsible for holding the teeth (alveolar bone). Oddly enough, individuals with this form of gum disease rarely form dental plaque or tartar.
3. Generalized Aggressive Periodontitis – typically begins around puberty and affects the entire mouth. Symptoms include swelling of the gingiva and excessive accumulations of tartar and plaque. Left untreated, this disease can cause loosening of the teeth.
To successfully treat periodontal diseases, early diagnosis is essential: Patients should receive a Comprehensive Periodontal Examination during their routine visits to the dentist. An advanced form of gum disease could be an early sign of another systemic disease; therefore, children exhibiting severe gum disease should visit their physician for a general medical evaluation.
How Can Periodontal Disease Get Treated?
Your dentist will take x-rays and examine your teeth and gums. Once you get a diagnosis, the dentist or periodontist will provide you with treatment that is dependent on the severity of your situation. There are various treatment options but the thing to remember is that along with the treatments it is very important for you to improve your oral care on a daily basis. This may require that you make some changes in your daily life including lifestyle changes such as quitting smoking and limiting your sugar intake.
What Is Deep Cleaning?
Deep cleaning is when the periodontist removes all of the plaque on your teeth and gums through a method known as scaling. Scaling involves scraping tartar above and below the lining of the gums. Root planning will also be done in this procedure to smooth out any rough spots where bacteria gather to stop the ailment from escalating any further. This will procedure may be done manually by a periodontist. Sometimes your dentist may use laser treatment that is more advanced. The laser treatment involves less swelling and bleeding. Some patients say that treatment lessens discomfort.
What Is Flap Gum Surgery?
Flap surgery is necessary is more advanced cases of periodontal disease. This type of surgery is for those who have undergone a deep cleaning treatment and did not see satisfying results such as persistent inflammation and deep gum pockets. Flap surgery is the surgical lifting of the flap (the gums) and removing any tartar found so that it is easier for the patient to keep the area clean.
What are Gum Disease Risk Factors?
Plaque is the principal reason that an individual develops gum disease; however, other factors can affect the health of the gums. Other risk factors include:
Tobacco use
studies indicate that tobacco may be a significant risk factor in developing gum disease: Furthermore, continued smoking causes gum disease to progress.
Age
According to the CDC, a little more than 70 percent of Americans who are 65 years or older have Periodontitis.
Genetics
It is believed that some individuals are genetically susceptible to developing gum disease.
Medications
Certain medicines can affect an individual’s oral health. These drugs include antidepressants, oral contraceptives and a variety of heart medications.
Stress
Just as stress has been linked to a variety of severe conditions (cancer, high blood pressure, etc.), it is a risk factor for gum disease as well.
Grinding or clenching the teeth
When an individual clenches or grinds his/her teeth, an excess amount of force is placed on the gums, which could increase the progression of gum disease by destroying the periodontal tissues at a faster rate.
Obesity
Research indicates that obesity may increase the likelihood that an individual will develop gum disease.
Poor nutrition
Since periodontal disease starts as an infection, anything that compromises the body’s ability to fight off infection increases the risk of developing periodontal disease.
Systemic diseases
Diseases such as rheumatoid arthritis and diabetes are known to alter the efficiency of the inflammatory system, these types of conditions may negatively affect the condition of the gingiva (gums).
What are the Symptoms of Gum Disease?
Unfortunately, gum disease is frequently silent until it reaches the advanced stages, which is why prevention through good oral hygiene is recommended. There are some warning signs once the advanced stage of gum disease is present:
- Gums that bleed while eating solid foods, flossing or brushing the teeth.
- Inflamed, red gums that are tender or any other type of pain in the mouth.
- Constant halitosis (bad breath).
- Loose teeth.
- Teeth that are changing position.
- Mouth sores.
- Changes in the way an individual’s teeth fit together when taking a bite.
- Pus is present between the teeth and gums.
- Receding gums that cause the teeth to look longer than they were before the gums started pulling away.
- Changes in the way that a partial fits.
Can Gum Disease be Prevented?
Yes, gum disease can be prevented through the practice of good oral hygiene, which includes:
- Flossing at least once daily to remove plaque and particles of food that a toothbrush is unable to reach.
- Brushing after meals helps in the removal of trapped food debris and plaque.
- The tongue houses bacteria as well, for this reason, the tongue must also be brushed.
- Discussing any of the risk factors (listed above) for developing the periodontal disease with his or her dental professional.
- Using mouthwash to reduce plaque and remove food particles missed when flossing, and brushing.
- Visiting a periodontist annually for a Comprehensive Periodontal Evaluation (CPE).
Parents can begin brushing their child’s teeth with a small amount of toothpaste once he or she turns 12 months old. Also, once the gaps between the child’s teeth close, flossing should be implemented.
Is Gum Disease Associated with Any Other Diseases?
Yes, previously, it was believed that bacteria played a role in linking gum disease to other diseases; however, research indicates that inflammation may be the contributing factor. Consequently, addressing inflammation may accomplish much more than just helping with the management of gum disease, it may also assist with managing other chronic conditions that cause inflammation. These conditions include:
Can Gum Disease Cause Heart Disease?
Scientists think that the swelling associated with gum disease may be the link between heart disease and periodontal disease. Furthermore, gum disease can negatively affect existing heart conditions. For this reason, individuals who are at an increased risk for infective endocarditis may need to receive antibiotics before dental procedures are performed.
It may surprise you to find out that the health of your teeth can be a significant indicator of how healthy the heart is. In fact, studies have shown that those with periodontal disease may be 1.5 to 2 times more likely than the general population to face fatal cardiovascular disease. By taking care of teeth today, not only do you add to your appearance and health of the mouth, you may be able to help your heart beat stronger—now and into the future.
What Is The Relation Between Gum Disease and Diabetes?
Individuals who are diabetic are at an increased risk of developing gum disease: Furthermore, if periodontal disease is present, it can increase an individual’s glucose levels, leading to diabetic complications. In fact, gum disease is frequently considered one of the complications associated with diabetes.
What is the Link Between Diabetes and Periodontal Disease?
Severe periodontal disease increases glucose levels, which places the body under the stress of high blood sugar. This increases the risk for diabetic complications over time. Research indicates that periodontal disease may make it more difficult for diabetics to control their glucose levels. Because diabetics are also more susceptible to infection, they are more likely to develop periodontal disease than non-diabetics. It has also been shown that diabetics with well-managed glucose levels statistically do not have more instances of gum disease than non-diabetics.
Research has demonstrated a link between diabetes and periodontal disease. Diabetics that do not have good control over their blood sugar have been shown to get the periodontal disease more often than diabetics who do have good control. The risks exist for children with insulin-dependent diabetes mellitus (IDDM) as well.
Part of the increased risk of diabetes is the result of thickening of the blood vessels. Diabetics with poor blood sugar control tend to experience a thickening of the blood vessels, which inhibits blood flow to the gums and bones in the mouth and makes the removal of waste products less efficient as well.
When you are diagnosed with diabetes, you quickly become aware of how drastically the disease can affect your health if left uncontrolled. Your doctor most likely told you about the risks to your heart, eyes, nerves and other organs should you fail to maintain good diabetic control. One health risk that many people with diabetes are unaware of, however, is the periodontal disease. These diseases of the gum and bone can lead to significant discomfort, pain and even the loss of teeth in later stages. And, as with all infections, periodontal disease can make it more difficult to control your blood sugar.
Diabetes and Gum Disease: If you or a loved one has diabetes, you probably know how important it is to control the disease. However, you may not realize the link between diabetes and gum disease. Periodontal disease is an inflammatory infection of the mouth. The best way to prevent gum disease is to maintain good oral health.
If you leave gum disease untreated, there may be damage to tissue and bone around the teeth—leading to tooth loss. Since people with diabetes are up to four times more likely to develop gum disease, it is especially important to stay on top of treatment. Another concern for diabetic patients is a bone loss because of more aggressive disease activity. Ultimately, this can lead to tooth loss and eventually the lack of proper nutrition.
Diabetes leads to a patient’s chance of gum disease occurring, but also gum disease makes it more difficult for diabetic patients to control levels of blood sugar so it can become a vicious cycle. Because of this, prompt treatment of any periodontal disease symptoms is important as it can eliminate infection and allow for metabolic control.
Are Other Oral Problems Linked to Diabetes?
Several other oral problems can result from diabetes, including cavities, dry mouth, and thrush. The same poor oral care that causes gingivitis can lead to cavities. Dry mouth can be a symptom of diabetes in people who are unaware they have the disease. Dry mouth is not only uncomfortable, but it also means that the saliva that protects the teeth and gums is not working as it should, which can lead to sores and infections.
Thrush is associated with diabetes due to the high glucose levels of diabetic saliva. Thrush thrives in such conditions. Thrush is a fungus that can be treated with medication. A dentist will be able to identify thrush and prescribe the right medication to eliminate it.
Can Diabetes Cause Bleeding Gums?
Bleeding gums are a sign of gum disease. While diabetes can certainly contribute to gum disease, it does not cause gums to bleed directly. You can have diabetes and never experience bleeding gums. Fortunately, good dental care and keeping your blood sugar under control is usually sufficient to prevent bleeding gums.
Can Diabetes Cause Sores in the Mouth?
Sores in the mouth can be caused by some factors, including dry mouth, ulcers, periodontal disease and other infections. Diabetes can be a contributing factor in these diseases and conditions, but diabetes does not cause mouth sores directly. You can help avoid mouth sores by controlling your blood sugar and practicing good oral care.
Can Bad Teeth Lead to Diabetes?
No, bad teeth do not lead to diabetes. The poor health habits that lead to diabetes can sometimes lead to problems with the teeth, but people with perfect teeth can still get diabetes. However, bad teeth can cause other health problems if left untreated. The infections that often come with bad teeth and gums need to be treated by a dentist as soon as possible to prevent further complications.
Can Diabetes Cause Tooth Loss?
Diabetes does not cause tooth loss directly. Diabetes can contribute to tooth loss, though, if diabetes helps to cause periodontal disease. Once periodontal disease sets in, it can lead to the loosening of teeth and eventually the loss of teeth as the support structures for the teeth – the gums and bones – are destroyed. Periodontal disease often does not exhibit any symptoms until is quite advanced, which is why it is vital to make regular visits to a dentist – especially if you have diabetes. The pain and lose teeth of periodontal disease only show themselves when the disease has progressed significantly.
Are There Any Factors That Increase the Risk of a Woman Developing Gum Disease?
Yes, there are several factors that increase a woman’s risk of periodontal disease:
-
Menstruation
Just before the onset of menstruation, some women experience bright red, inflamed gums that bleed as well as sores on the inside of their cheeks. This form of gum disease is referred to as ‘menstruation gingivitis.’ This condition usually begins directly before the period begins and clears up as soon as menstruation starts.
-
Pregnancy
A woman who is pregnant and has periodontal disease may be putting her baby at risk. Periodontal disease may cause the baby to be born too early and be too small; however, this link has yet to be firmly established, and more research is necessary to confirm this relationship. Since every infection is of concern during pregnancy, women who are pregnant or are considering pregnancy should have a Comprehensive Periodontal Evaluation.
-
Puberty
An increase in the level of estrogen and progesterone during puberty causes an increase in blood circulation to the gums. This additional blood flow may increase the sensitivity of the gums; thus, leading to a greater response to irritations, including plaque and food particles. As such, the gums may appear red and inflamed.
-
Menopause/Post-Menopause
During and following menopause, women may notice changes in their mouths. These changes may include burning sensations, pain in the gum tissue and on the tongue. Other symptoms include a dry mouth and an altered taste (sour, peppery or salty). Additionally, some women experience shiny or dry-looking gums that bleed easily and appear either abnormally pale, or deep red in color. This condition is referred to as menopausal gingivostomatitis. Typically, estrogen supplements successfully relieve these symptoms.
What are other oral problems linked to diabetes?
If diabetes is poorly managed, high glucose levels in saliva promote bacterial growth. This creates the perfect environment for gum disease to develop. These are some of the other oral problems caused by diabetes:
- Thickened blood vessels – Diabetes thickens blood vessels, reducing the flow of oxygen and nutrients to tissue. This weakens the resistance of gum and bone tissue to infections and increases the potential for gum disease.
- Thrush – Thrush is an oral fungal infection and diabetics have a higher risk for it due to high glucose levels in their saliva. It causes white or red patches on the skin of the mouth which can result in discomfort and ulcers.
- Dry mouth – Dry mouth can be a symptom of undetected diabetes and cause ulcers, infections, soreness and tooth decay.
- Cavities – It might seem diabetic children are more susceptible to cavities. This is not the case. They have no more tooth decay than nondiabetic children and often have fewer cavities since they eat less sugary foods.
- Bleeding gums – Red, sore, bleeding gums are warning signs of early gum disease.
- Gum recession and tooth loss – A Severe periodontal disease can cause changes in bone shape and gum tissue, leading to painful chewing problems and complications, especially for denture wearers.
A recurring theme with these conditions is that good diabetic glucose control can prevent many of them.