What you need to know before a root canal treatment

When a tooth has become infected or severely decayed, it can cause severe pain and swelling. In these cases, patients have two options: extraction of the tooth or a root canal treatment. Extracting a tooth can cause several potential complications, including difficulty chewing, shifting of other teeth, and TMJ pain caused by a change in the bite.
Before you decide between root canal treatment or teeth extraction, you need to know about these five factors about root canal:
Table of Contents
Why do you need root canal treatment?
If one of your teeth is infected, because of decay or trauma to the tooth, root canal treatment is the most comfortable and most affordable option to save the tooth. A root canal is most often the treatment of choice to preserve the natural tooth. A root canal is typically less painful than extraction and carries a shorter recovery time. Most patients state that root canal pain is very similar to the discomfort experienced when having a tooth filled.
How Do I Know if I Need A Root Canal?
To know more about the root canal, read our previous articles about root canal signs and symptoms. You will not know until you see an endodontist to be diagnosed. The symptoms mentioned above of pain in the tooth and jaw, Inflammation of the gums, and prolonged sensitivity could be the result of other conditions. Your endodontist will take X-rays and examine your teeth and gums to determine the best course of treatment.
What Are The Root Canal Problem Symptoms?
You may need a root canal if:
- Temperature-sensitive tooth pain – teeth are very sensitive to hot and cold for a prolonged period
- Gums are tender and swelling
- Jaw and toothache
How is a root canal procedure done?
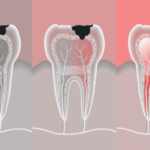
To understand the root canal treatment procedure, you need to know the anatomy of the tooth. The part of your tooth that extends past the gums and is visible to the naked eye is called the crown. The soft center of your tooth is referred to as the pulp chamber while inside the root of your tooth is known as the root canal, which extends from the tip of the root into the pulp chamber and contains the nerve of the tooth. Both the pulp chamber and the root canal are filled with connective tissue and blood vessels that provide nourishment to the tooth.
Decay that is limited to the crown of the tooth can typically be treated with a filling, but decay that has reached the pulp chamber or the nerve of the tooth requires root canal treatment. An abscess, which is a pocket of pus at the tip of the root that can occur with or without tooth decay, usually produces severe pain and must be treated with a root canal. A tooth can function with or without the nerve, making root canal treatment a viable option for saving your tooth.
During root canal treatment, your dentist will remove the infected nerve and pulp from the root canal system, seal it with a biocompatible material called Gutta Percha. Incisors and canines typically have a single root and a single canal. Premolars usually have two, and molars have three or four canals. Root canal treatment relieves the pain of an infected or abscessed tooth.
In the days and weeks, before you find out you need a root canal, the primary symptom is most often a severe toothache. If your tooth becomes infected, you may notice sudden swelling of one side of your face.
Both dentists and endodontists can perform root canal procedures. Endodontists are dentists who specialize in the diagnosis and treatment of injuries and diseases to the pulp or nerve of the tooth. Your dentist will help you decide who should perform your root canal based on several factors, including your dentist’s level of comfort in performing the procedure in your case and the difficulty of your specific root canal procedure. Curved or narrow tooth canals can make a root canal procedure more difficult.
When you arrive for your appointment, the dental staff will take an x-ray of your tooth. Taking an x-ray allows the endodontist to determine the shape of your root canals and the status of the bone surrounding the tooth.
Next, your dentist will apply local anesthesia to numb the area surrounding the affected tooth. A rubber dam is placed around the tooth to prevent saliva from coming in contact with your tooth during the root canal treatment.
Your dentist will test your level of feeling to ensure you’re numb enough to begin the procedure.
The root canal itself takes around 30-90 minutes, depending on the patient’s individual needs and the doctor’s experience. The procedure involves six significant steps
- A local anesthetic will be applied to the nerves that lead to the tooth.
- A rubber dam will be placed around the tooth to keep the area clean during the treatment
- A small hole will be drilled into the tooth.
- The infected pulp will be removed.
- The root canal space is disinfected.
- The Endodontist will then fill the root canal space with a biocompatible material called Gutta Percha. The access cavity will be cover with a temporary material and is referred to as the general dentist for the permanent restoration.
Nickel-titanium files, increasing in diameter with each step of the process, are inserted one by one into the root canals of the teeth, removing the pulp, connective tissue, blood vessels, and the nerve of the tooth. Your endodontist will also use EDTA, sodium hypochlorite, and Chlorhexidine to wash away bacteria and debris during the process.
Your dentist will now fill the pulp chamber and root canals with a rubber compound and sealer paste and fill the cavity he or she created to access the inside of your tooth. In most cases, tooth restoration such as a crown is required following root canal treatment due to significant decay.
Is it normal to have pain after root canal treatment?
If you were in pain before your root canal, you should notice that the pain is relieved significantly following your procedure. You may notice that the tooth is sensitive in the days following your treatment; this is a normal response to inflammation in the tissue surrounding the tooth and can be managed with over the counter anti-inflammatories and pain relievers.
You should not chew on the tooth being treated until treatment is complete to avoid breaking the tooth. If you have another appointment to cement a crown, avoid chewing on the tooth until after your crown is seated. At all stages and after treatment is complete, continue to brush and floss twice daily and see your dentist regularly for prophylactic cleaning and exam.
What is the success rate of root canal treatment?
Root canal treatment has a 95% success rate. In some cases, a crack in the root of the tooth or an inadequate restoration can cause infection to return to the tooth. In these cases, an endodontist can usually perform root canal retreatment or apicoectomy to relieve pain, treat the infection, and save the tooth.
There are many elements for success in endodontic treatment — starting with making a correct diagnosis. First, we attain access, providing an opening to view root canal orifices and the root canal system. Then, the preparation of the root canal is directed toward the objective of cleaning and shaping. Studies have shown that file shape, and irrigation cleans the root canals. By shaping first, cleaning is more comfortable, and both steps make for better filling. After that, condensation gutta-percha and sealant into the root canal system to provide obturation. After the root canal treatment, dentists will restore the teeth to provide aesthetic appeal and achieve a coronal seal.
What is the cost of root canal treatment?
The average root canal costs around $800.00 without insurance, with the back teeth being the most costly. They range between $500-$1400 per tooth. In addition to the tooth to be treated, costs can vary based upon:
- Location (Cost of living is higher in some parts of the country)
- Crown materials requested – Non-Gold Metal, Gold Metal, Porcelain-Metal Fusion, etc.
- Condition of the tooth
Is Root Canal Painful?
The root canal treatment itself is a pain-free procedure. Everyone feels pain differently, so no one can say that you will feel no pain. But it is important to realize that a root canal relieves pain; it does not cause it. The inflammation and infection cause a toothache, not the root canal treatment. Most of the time, patients’ anxiety and expectation of pain are much higher than actual pain.
How Do I Reduce Root Canal Pain After The Treatment?
There are several methods commonly used to treat root canal pain after the procedure. They include:
- Ibuprofen (relieves pain and reduces swelling)
- A local numbing agent like “Orajel.”
- A cold compress (a bag of unopened frozen vegetables that you do not intend to eat works well)
- Salt Water (soothes irritated gums and also reduces the chance of infection)
Root Canal Recovery
During the first week after the root canal, you should experience gradual healing and begin feeling well enough to start resuming normal activities very soon after the procedure. If you do not feel that you are getting better after a week, then you should contact your endodontist.
What Is A Root Canal Infection?
In rare cases, the infection from the tooth that has been treated may spread throughout your mouth and into your bloodstream. This could make you very sick and even result in hospitalization. Do not disregard Doctor’s Orders related to personal care after the procedure to avoid such complications.
What is the difference between Endodontist & Dentist?
“Endo-” means “inside” and “-dontist” means “one who treats teeth.” An endodontist is a doctor who specializes in the treatment of the inside of the tooth. He or she may undergo up to 2 years of additional training specifically to provide endodontics procedures.
The most common procedure related to the inside of the tooth is the root canal. Because the endodontist may perform 20-30 root canals a week, compared to a dentist who may do 2-3 a week, the endodontist is typically able to provide a better root canal experience because of this additional training and constant practice.
Are There Any Alternatives to A Root Canal?
The root canal is designed to save the tooth. In some cases, a person may opt to have the tooth extracted instead. To make this decision, you will want to consult with your doctor. Read our previous article about pulp regeneration for more information about root canal alternatives.
Here are some things to consider when making this choice.
- You may prefer implants or another solution to resolve the issue
- You and your doctor may decide that, based upon your oral history, extracting is a better option for you.
When a tooth is extracted, you may choose to replace the tooth with a:
- dental implant
- bridge
- partial denture
Is It Better to Get a Root Canal or Dental Implants?
Significant research has been completed on the topics of root canal vs. dental implants. Endodontic procedures are equally effective as dental implants when it comes to treating and restoring the natural appearance and function of the teeth.
Why do endodontically treated teeth sometimes fail, and what causes this?
There are different causes of root canal treatment failure. Microleakage and bacterial infection can be a big problem. Root canal treatment failure can be attributed to issues with the cleaning, shaping, or root canal filling. Other problems can include missed canals, root fractures, iatrogenic events, or reinfection of the root canal system when the coronal seal is lost. The main cause overall is a bacterial infection, no matter what the source.
What Happens if My Root Canal Fails?
A root canal is said to “fail” when it becomes re-infected or cannot be completed due to complications.
This may be the result of:
- Failing to maintain oral hygiene
- A crack or leak to the crown that is placed over the treated tooth
- The presence of an extra canal – some people have a tiny, extra canal that goes undetected and untreated
- An inability to properly navigate the canals
- An endodontic tool becoming lodged in the canal while trying to navigate difficult canals.
If the failure happens during the procedure, your endodontist will take proper steps to achieve the best outcome for you as a patient despite the complication.
If the failure occurs after the procedure, unfortunately, because the root canal itself removes the pulp within the canal along with the nerves and blood vessels inside it, you are unable to feel that anything is wrong until significant damage has occurred.
Regular visits to your Dentist and Follow-ups with your Endodontist allow for early detection when the root canal is subject to failure. Failures are more common in back teeth because they have more roots, more curved roots, and they are harder to clean and treat.
With the above said, a root canal performed by a trained and experienced endodontist has around a 95% success rate, which is considered very high.
What is Re-treatment of A Root Canal?
In the rare occasions when a canal is missed, or there is a fracture or break in the seal, the patient may need endodontic surgery. Endodontists use state of the art technology and endodontic treatment to save the tooth despite the root canal failure.
Among these procedures, the most common is called an “apicoectomy” in which the endodontist:
- Administers a local anesthetic to reduce pain and discomfort
- Resects (pulls back) the gums to access the roots
- Removes the inflamed and infected tissues
- Places a small filling to seal the root and prevent further infection
- Stitches up the gums to allow the area to heal
This procedure sounds complex, but it is minimally invasive, and the healing time is typically short.
What is the success rate for endodontic retreatment?
It has been reported excellent results—around an 85% success rate. Dentists can retreat nearly all failures with non-surgical means. In the other 15% of cases, apical surgery, or tooth extraction is required. The higher failure rate in retreatment is due to the need to overcome a number of other existing problems.
Since root canal retreatment addresses several circumstances to achieve success, what are some of the most important to make root canal retreatment a success?
Endodontic retreatment usually involves accessing the canals through restoration—so there must be an effort to remove or work through that. Then, the core materials need to be removed from the pulp chamber. After this, the pulp chamber is inspected for missed canals. Then, root canal retreatment involves removing posts and cores and obturation materials. There may be more work needed than usual negotiating blocked canals or working on issues involving perforations, apical transportations, and ledges. Once the root canal has been negotiated and shaped, they are packed, and the process is completed, much like it is done for first-time treatment.
Related articles: