Recent Posts
Tooth Abscess
Moderate to serious tooth pain can indicate the presence of an abscessed tooth, sinus infection, or infection at the root of your tooth. You could feel significant pain when you chew, be sensitive to hot and cold temperatures and notice redness and swelling in your gums. While it doesn’t have to be painful, a tooth abscess should be treated by a dentist right away or it could develop into an emergency.
Table of Contents
What is an Abscessed Tooth?
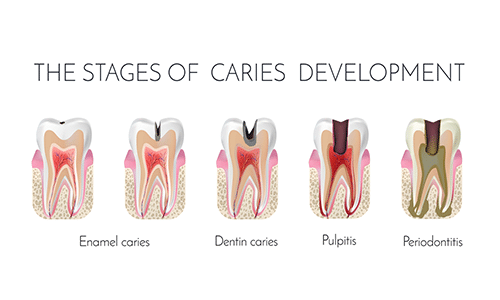
The inner chamber of each tooth contains pulp, a soft tissue filled with blood vessels and nerves. A crack in your tooth can give bacteria a foothold into this area, and the sensitive tooth pulp can become infected. Often, the infection gets worst at the root of the tooth, deep down inside your gum. When infection develops, your body sends white blood cells to fight off the invading bacteria. A byproduct of this fight is pus, a thick fluid that contains dead tissue and bacteria. The pus forms inside the tooth and, with nowhere to go, often ends up forming a pocket at the root of your tooth – though it’s possible for an abscess to form anywhere along the tooth. This pus puts pressure on all the sensitive nerve endings in the tooth pulp and gum, leading to the pain and discomfort you’re feeling. Another type of problem infection comes from what’s termed a “dry socket.” When a tooth is pulled, a clot forms over the empty spaces as the gum heals. Occasionally, infection starts and an abscess forms in the empty tooth socket when that clot gets dislodged or dissolves. The exposed nerves make this condition especially painful. Only a couple of centuries ago, dental abscesses were a leading cause of death. With today’s antibiotics and modern dental treatments, far fewer people die from infections in their mouths, but it can still happen, like in these cases:
- A 26-year-old truck driver from Sacramento died in 2017.
- A 24-year-old unemployed dad from Cincinnati died in 2011.
- A 12-year-old boy in Maryland died in 2007.
In fact, a Boston study found that the number of people hospitalized for dental abscesses increased by more than 40 percent between 2000 and 2008, and of those patients, 66 died. In other words, an abscessed tooth is not only a source of pain or a sign that your oral health isn’t what it needs to be – it’s a medical emergency that must be treated as quickly as possible.
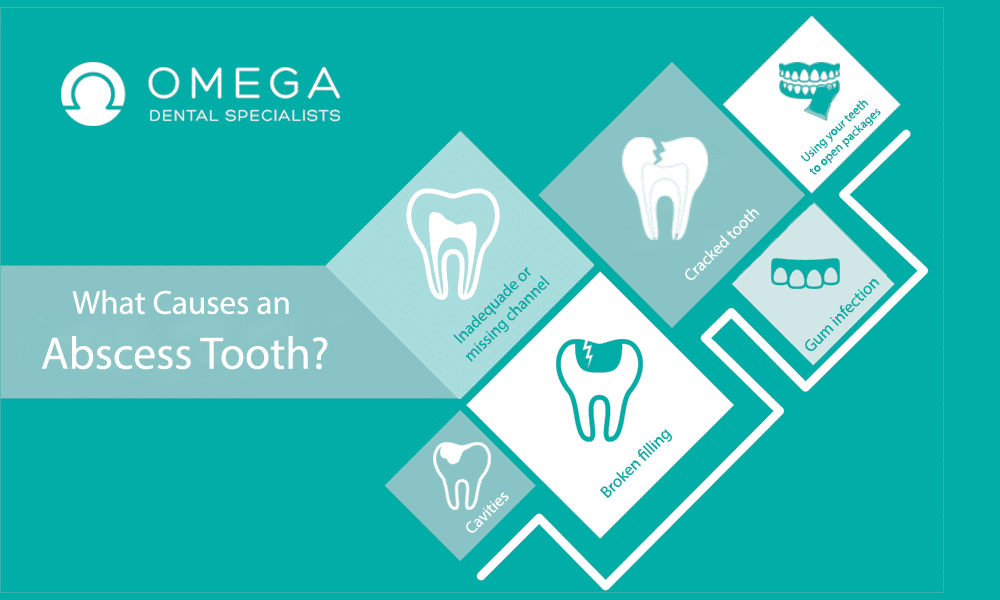
What Causes an Abscess Tooth?
Any circumstance where oral bacteria can enter the tooth or get deep below the gumline can lead to a dental abscess. Top causes include:
- Untreated tooth decay, otherwise known as cavities or caries
- A cracked tooth
- A dislodged, chipped, broken or missing filling
- A root canal where some tooth pulp was left, called an inadequate or missed canal
- A gum infection, like what you’d experience with advanced periodontal disease
- Using your teeth or mouth as a “tool” to open packages or cut wire; this could cause a puncture that allows bacteria to enter
Sometimes it’s not obvious exactly how an abscess was caused. If the cause might have been related to an issue with your oral health, your dentist can help you make changes to reduce the risk of getting another dental abscess. Scheduling regular preventative dental appointments and maintaining good oral hygiene are important habits to develop in order to keep from developing dental abscesses and other oral health problems.
How Is an Abscess Tooth Diagnosed?
Based on your symptoms, your dentist can usually diagnose an abscess tooth based on your symptoms and the appearance of the tooth and gum. You may be asked if you have any of these signs:
- Throbbing pain in your jaw, neck or ear
- Swelling in your gums
- Sensitivity to hot and cold temperatures
- Sensitivity to pressure
- Signs of infection like swollen lymph nodes and fever
Your dentist may perform a manual exam that includes visual confirmation of some or all of the symptoms, including gentle tapping on the affected tooth to check sensitivity. If all signs point to a dental abscess, you may need an X-ray, which can usually show the pocket of infection and whether it has spread. Rarely, an X-ray may not be definitive or the infection may have spread throughout your head or neck, and a CT scan will be needed to pinpoint the issue.
How Is an Abscessed Tooth Treated?
Because an abscessed tooth and the resulting infection can be life threatening, it’s important to tackle the infection quickly. The first step in treatment is to administer antibiotics. These antibiotics can quell the infection and keep it from spreading, but you’ll still require a dental procedure to permanently treat the area of the abscess and keep it from returning. If you’re allergic to amoxicillin, which is the first line of defense against infection, your dentist will prescribe Clindamycin. To reduce pain and swelling, your dentist may recommend a minor surgical technique to drain the abscess. Reduced pressure will help alleviate your pain until the right permanent treatment is determined. However, a larger abscess which has spread to your mouth or neck may require anesthesia and a more involved surgery. The cost of this procedure depends on how complicated the surgery is and whether it can be performed in your dentist’s office. After acute care, you’ll have to decide on a permanent treatment for the damaged tooth — or the infection cycle will start all over again. Your dentist will likely recommend one of two options:
Root Canal
A root canal is the best way to save your tooth and prevent future infection. More than 15 million root canals are performed each year; it’s a common procedure that is typically performed on an outpatient basis by a general dentist or a dental specialist called an endodontist. Most people choose root canal over extraction so they don’t lose the tooth. During a root canal, the dentist or endodontist will remove the diseased pulp tissue inside the tooth and drain the abscess. Very small tubes within the interior of the tooth, called canals, must be cleaned out completely so infection can’t return. The empty pulp chamber and canals are then filled with a non-toxic dental compound to strengthen the tooth. In order to successfully perform a root canal, the tooth must be in good condition without significant decay or cracks. Depending on complexity, a root canal will usually cost between $800 and $1,500. Once the procedure is completed, the tooth will be strong enough to chew with, just like before you had the abscess.
Tooth Extraction
In a tooth extraction, the affected tooth is removed completely so the abscess at the root can properly drain and heal. Because abscesses are often caused by damaged or cracked teeth, this might be only reasonable solution to prevent future problems. Tooth extractions are recommended when the tooth is too damaged to successfully perform a root canal. Once the tooth is extracted and the abscess has completely healed, your dentist can evaluate the possibility of a bridge or even an implant to replace the extracted tooth. Tooth extraction starts at $300 for a simple procedure; bridges can cost between $500 and $1,500. Ask your dentist about other options for tooth replacement. As each case is unique, your dentist can work with you to create a customized plan for dental abscess treatment. If cost is a factor in your decision, your dentist’s office can present options and suggest possible payment plans that may make finances less of a concern.
Can an Abscess Tooth Be Prevented?
Practicing good oral health care can significantly reduce your risk of developing a dental abscess. Sometimes, even those patients who take very good care of their teeth and schedule regular dental appointments for preventative care will get an abscessed tooth, but it’s rare. Here’s how to minimize your risk of an abscess:
- Brush and floss regularly to reduce harmful oral bacteria.
- Use products with fluoride to strengthen your teeth.
- Eat a diet low in sugary foods and high in nutrients to help maintain healthy teeth.
- Stay away from cigarettes, chewing tobacco and other tobacco products.
- Avoid using your teeth as a tool to open packages, strip wires or cut through cords.
- Schedule regular dental visits, and see your dentist immediately if you crack or chip a tooth.
Establishing good dental health habits not only prevent abscesses, but will keep your teeth from developing caries and decay that cause a wide range of dental diseases.
What Specialists Might You See During Your Treatment for an Abscess Tooth?
In addition to your regular dentist, who will likely evaluate and diagnose your abscess, you may need to schedule an appointment or surgery with an endodontist. Endodontists specialize in treating infected pulp in a diseased tooth, usually through root canal. In all but the most simple cases, you’ll want to work with an experienced endodontist if you do decide on root canal surgery. If any pulp is left in the tooth or the tooth is not sealed properly, bacteria can gain access and start the whole cycle of abscess again. A skilled endodontist can ensure the root canal is performed correctly and your mouth is able to heal. We work with and are able to recommend qualified endodontists if you do need a root canal.
What Are Your Other Health Risks When You Have an Abscess Tooth?
If you don’t get treatment for an abscessed tooth, you’ll be at risk of other serious — in some cases, life threatening — issues, such as:
- Tooth loss. Early treatment may mean you can save your abscessed tooth. If you wait, it’s much more likely it will need to be extracted. If infection spreads, you may lose more teeth.
- Bone infection. Jaw bones are typically more fragile than other, larger bones in the body. Infection can cause large holes in the maxilla and mandible, which may then need to be removed completely. This can impact your appearance and your ability to chew.
- Sinus infection. Not only your sinuses can be impacted, but the other soft tissues in your face can become inflamed. This may lead to facial disfigurement and respiratory issues.
- Sepsis. Infection from a dental abscess can erupt and spread to your bloodstream, and from there, throughout your body. Once you have an infection of this type, your life is at risk. You may require extensive hospitalization and antibiotic treatment for this type of blood infection.
- Endocarditis. Infection can spread from your mouth to your heart tissue, which leads to damaged heart valves and an increased risk of coronary artery disease.
- Brain infection. If infection spreads to your brain, it can be very difficult to treat and is also potentially fatal.
In short, don’t wait to get professional dental treatment for an abscess. The risks are simply too high to wait.
Can an Abscess Tooth Go Away on its Own?
What if you just wait and bear the discomfort of a tooth abscess? Will the abscess eventually go away? Sometimes patients, especially those without dental insurance or with very limited coverage, will wait to see a dentist even when they know there’s a problem. Honestly, an abscess tooth may go away in some isolated instances. But if it doesn’t, it will spread to your face and neck, turning a simpler treatment into an extremely complicated surgery. And you’ll be at risk of the very dangerous conditions described above. It doesn’t make financial sense to wait for treatment if you suspect an abscess. Call your dentist’s office and ask about payment plans and other options available to you, rather than hoping it will get better. An abscessed tooth rarely goes away on its own and usually develops into a costly medical emergency if not treated right away.
November 06, 2019Use Endodontic Microscope in Contemporary Endodontics
November 10, 2018
Is It Possible to Fix a Cracked Tooth?
November 10, 2018
Is There an Alternative to Root Canal Treatment?
October 31, 2018
Can Root Canal Cause Sinus Infection?